Procedures
|
Carotid stenting- to treat carotid arteries not amenable to surgical treatment |
|
EECP (Enhanced External Counter-pulsation) |
Cath / PTCA / Stent
Cardiac catheterization, also known as a coronary angiogram, is an invasive diagnostic procedure that assesses the heart's arteries, valves, and contractility (squeezing strength of the heart muscle) as well as the pressures generated within the heart and lungs. Tiny tubes called catheters are inserted through the groin or arm vessels under X-ray (fluoroscopic) guidance while you lie flat. Dye is injected into the heart arteries to determine if there is blockage and into the main pumping chamber of the heart to determine its strength, known as the "ejection fraction". Local anesthesia is given at the insertion site and oftentimes a light conscious sedation is used. If the groin approach is used, you may need to lie flat for several hours to allow the puncture site to heal. Catheterizations are performed both on inpatients and outpatients.
Following cardiac catheterization, your physician may advise medication, balloon angioplasty, or surgery.
Percutaneous Transluminal Coronary Angioplasty, known as PTCA, is the procedure that uses a balloon to open a blocked artery. After a thin wire is passed across a blockage, a balloon-tipped catheter is inflated, flattening the plaque against the artery. Blood thinners are given during the procedure, and the tiny tubes inserted in the groins, called sheaths, may not be removed for several hours until the blood thinners lose their effect. Because there is a small risk of needing emergency surgery for failed angioplasty, the procedure is performed at the hospital on an inpatient basis.
Unfortunately, the angioplasty technique is plagued with up to a forty percent (40%) recurrence of the blockage, often within the first six months. This recurrence is known as restenosis. Coronary stents are small metallic scaffolds, often balloon -mounted, that are permanently placed across a blockage. Stents are known to reduce restenosis to less than twenty percent (20%) in many cases.
Rotational Atherectomy, or Rotablator®, is often done in conjunction with PTCA and stenting. A small high-speed drill is passed over a wire to pulverize plaques into microscopic particles. Rotablator® is particularly useful for small, diffusely diseased arteries, and arteries with heavy calcium deposits. Directional Atherectomy, called DCA, uses a small cutting blade to shave plaque into a chamber. The debris is then removed from the body. Large, bulky blockages respond well to DCA.
Intravascular Ultrasound, or IVUS, is essentially an echocardiogram performed on a catheter placed within the artery. It gives information on vessel size, plaque composition and percent stenosis. Intravascular ultrasound is used to ensure the proper seating of stents against the arterial wall.
Peripheral angioplasty, called PTA, is the balloon technique applied to the peripheral arteries. Peripheral stents are placed in selective locations. Renal artery angioplasty and stenting are used for treating blockages of the kidney arteries. This may help preserve kidney function or decrease the high blood pressure caused by these blockages.
Patient Preparation:
-
No food or drink at least four (4) hours before the procedure.
-
Take your medications with sips of water unless otherwise instructed.

Echocardiograms
An echocardiogram is a noninvasive, painless, test that uses ultrasound (high frequency sound waves) to produce a two dimensional image of the heart. As we view the beating heart on a television monitor, we can measure heart chamber sizes and wall thickness, assess the strength of the heart and examine its structure, including the heart valves. Color flow and Doppler techniques use ultrasound frequencies to measure the degree of valvular obstruction (stenosis) or leakage (regurgitation or insufficiency).
Echocardiograms are commonly ordered to evaluate heart murmurs, palpitations, chest pain and valvular abnormalities. They are essential tools for understanding congestive heart failure.
Stress echocardiograms combine stress testing, either with treadmill exercise or with intravenous Dobutamine, and an echocardiogram. The stress-echo combination can shed further information on specific regions of the heart muscle or the heart valves when your body demands increased blood flow.
The transesophageal echocardiogram is a more invasive procedure during which you are lightly sedated to help you swallow a probe that is attached with an echocardiogram transducer. By imaging from the esophagus (passage leading from the mouth to the stomach), we reduce the tissue thickness that exists between the chest wall and the heart, and are able to produce more detailed echo images.
Patient Preparation:
-
No special preparations are necessary for routine echocardiograms. Allow up to one hour.
-
Stress echocardiograms require no food or drink four (4) hours before the test.
-
Transesophageal echocardiograms require fasting from the previous night.
-
Routine medications should be taken for all types of echocardiograms.

Electrophysiology / Arrhythmias
Electrophysiology, or EP, is the branch of cardiology that deals with the electrical system of the heart including rhythm disturbances, called arrhythmias. The normal electrical or conduction system includes a natural pacemaker called the SA (sinoatrial) node that sends impulses to the AV (atrioventricular node) which then distributes the electrical charge to the main pumping chambers of the heart via the bundles. A malfunction or short circuit at different locations along the conduction system can lead to fast arrhythmias known as tachycardias, or slow arrhythmias, known as bradycardias.
Holter monitors and event monitors record your heartbeat during daily activities. The Holter monitor records all your heartbeats, usually over a 24-hour period. Event monitors record selected rhythms that correlate with your symptoms, usually over a two week interval. Both monitors are roughly the size of a calculator. The monitors are often ordered for complaints of palpitations, dizziness, or passing out.
Patient Preparation:
-
No special preparations are necessary. Because of its electrical circuitry, it is recommended that you shower before a Holter monitor is applied.
Cardioversion is the inpatient procedure attempting to convert an irregular heart rate, usually atrial fibrillation or atrial flutter, to a normal rhythm, either with medication or an electrical shock. A light anesthesia is given during electrical cardioversions. Following cardioversion, your physician may elect to start new antiarrhythmic drug therapy that may require several days of inpatient monitoring. Atrial fibrillation and atrial flutter are "quivering" rhythms of the upper heart chambers. If they persist beyond 48 hours, they require several weeks of anticoagulation with Coumadin to reduce the risk of stroke before cardioversion is attempted.
Permanent pacemakers are placed for bradyarrhythmias (slow heart rates). Sometimes the pacemaker completely controls the heart rhythm, at other times it only serves as a backup for slow rates. Pacemakers consist of two parts: the generator and the lead(s). The generator stores the pacemaker battery. It is roughly the size of a silver dollar and is usually surgically inserted under the skin near the collarbone. One or two thin wires, called leads, are threaded through the veins to the right heart chambers under x-ray guidance. After 5-8 years, the battery may deplete, requiring a new generator. The leads are usually left intact. Some restrictions are placed on you for a few weeks after a pacemaker insertion to allow the wound to heal and the leads to settle in place; then you can resume usual activities.
Several of the procedures listed below require the skills of a highly trained cardiologist, the electrophysiologist.
A sudden loss of consciousness is termed syncope (passing out). Two of the more common cardiac causes of syncope include arrhythmias and a condition known as neurocardiogenic syncope. The latter term describes abnormal nerve firings from the brain that lower blood pressure and heart rates leading to a sudden blackout spell.
Tilt table testing is used to assess neurocardiogenic syncope. An adrenaline type medicine is infused intravenously while you are strapped to a table that is raised to an 80 degree angle. A positive test will reproduce your symptoms. Tilt table testing is safe; it is often done in the office.
The electrophysiology study (EPS) is the electrical equivalent of cardiac catheterization. Catheters are inserted through the groin veins into various regions of the heart. These catheters can both sense electrical impulses and deliver electrical stimuli to reproduce various arrhythmias. The procedure is especially useful for sustained arrhythmias, as part of syncope workups, and for evaluation of cardiac arrest. Following an EPS, your physician may recommend medication, a pacemaker, an implantable defibrillator, or radiofrequency ablation.
Implantable defibrillators (ICD's) (photo above) are similar to pacemakers except they function to shock the heart during tachyarrhythmias, such as ventricular tachycardia or ventricular fibrillation. If left alone, these fast heart rates from the bottom chambers of the heart (ventricles) can be lethal. The newer defibrillators now also include a backup pacemaker.
Radiofrequency Ablation (RF) is sometimes performed in conjunction with an electrophysiology study. Certain arrhythmias can be cured or greatly reduced in frequency by the application of radio-frequency energy through a catheter. A small scar is created in the heart; this usually does not cause problems. Occasionally a pacemaker is required after an ablation.
Patient Preparations for cardioversion, pacemakers, tilt tables, EPS, defibrillators, and ablations:
-
No food or drink the day of the procedure.
-
Take your medications with sips of water unless otherwise instructed.

Stress Tests
A stress test, sometimes called a treadmill test or exercise test, helps a doctor find out how well your heart handles work. As your body works harder during the test, it requires more oxygen, so the heart must pump more blood. The test can show if the blood supply is reduced in the arteries that supply the heart. It also helps doctors know the kind and level of exercise appropriate for a patient.
A person taking the test
-
is hooked up to equipment to monitor the heart.
-
walks slowly in place on a treadmill. Then the speed is increased for a faster pace and the treadmill is tilted to produce the effect of going up a small hill.
-
may be asked to breathe into a tube for a couple of minutes.
-
can stop the test at any time if needed.
-
afterwards will sit or lie down to have their heart and blood pressure checked.
Heart rate, breathing, blood pressure, electrocardiogram (e-lek"tro-KAR'de-o-gram) (ECG or EKG), and how tired you feel are monitored during the test.
Healthy people who take the test are at very little risk. It's about the same as if they walk fast or jog up a big hill. Medical professionals should be present in case something unusual happens during the test.
A physician may recommend an exercise stress test to:
-
Diagnose coronary artery disease.
-
Diagnose a possible heart-related cause of symptoms such as chest pain, shortness of breath or lightheadedness.
-
Determine a safe level of exercise.
-
Check the effectiveness of procedures done to improve coronary artery circulation in patients with coronary artery disease.
-
Predict risk of dangerous heart-related conditions such as a heart attack.
Depending on the results of the exercise stress test, the physician may recommend more tests such as a nuclear stress test or cardiac catheterization.

Nuclear Stress Tests
There are four types of Nuclear Stress Tests:
-
1. Exercise Cardiolite Stress Test
-
2. Adenosine Cardiolite Stress Test
-
3. Dobutamine Cardiolite Stress Test
-
4. Lexiscan Cardiolite Stress Test
What is Cardiolite?
Cardiolite is a nuclear radioactive isotope termed Technetium Tc99m Sestamibi.
Cardiolite is injected through an IV and it travels in the bloodstream and through
the coronary arteries until it is picked up by the heart muscle cells. The areas of
the heart that have an adequate blood supply pick up the tracer right away and more
completely. Areas that do not have adequate blood supply pick up the tracer very
slowly or not at all.
Cardiolite gives off a small amount of radiation that is detected with a nuclear
scanning camera. A computer processes the information and produces the images of the
radioactivity distributed in the heart.
If an area receives less blood than the rest of the heart (because of a blocked or
narrowed artery), it will pick up a lower level of radioactivity and will show up as
a lighter area, called a "defect."
Cardiolite is injected while you are at rest and while your heart is under stress.
Rest and stress images are taken to allow doctors to compare how much blood flows
through the heart muscle during stress and at rest.
The amount of radiation you will be exposed to is comparable to that from an X-ray
or CAT (CT) scan. The half-life of Cardiolite is 6.02 hours. This means that half of
the dose you are given will decay in 6.02 hours.
Generally, Cardiolite is cleared from your body in 24 hours by natural processes.
You won't feel any different after you are injected with Cardiolite. Most patients
experience no side effects. Occasionally patients have a metallic taste in their mouth.
What is a Cardiolite Stress Test and what does it show?
A Cardiolite Stress Test is a diagnostic nuclear imaging study that uses a radioactive
tracer, called Cardiolite, to produce images of the heart muscle. When combined with
stress either through exercise or use of a pharmacological agent, the Cardiolite scan
helps determine if the heart muscle is getting the blood supply it needs.
As Coronary Artery Disease (CAD) progresses, the heart muscle may not receive enough
blood when under stress (for example, when exercising). This often results in chest
pain called Angina Pectoris. On the other hand, there may be no outward physical signs
of the disease. If CAD is limiting blood flow to part of your heart, the Stress Test
with Cardiolite may be useful in detecting the presence and significance of CAD.
A Cardiolite Stress Test consists of two parts, rest and stress:
Cardiolite will be administered by injection through your IV while you are at rest, and a special camera will take pictures of your heart.
Cardiolite will be administered to you one other time by an IV injection during the stress portion of the test, and additional pictures will be taken of your heart.
This allows the doctor to compare the amount of blood flowing through the heart muscle during stress and at rest.
How do I prepare for the test?
Do not eat or drink for 4 hours prior to the test--this includes caffeine! The pictures of your heart are clearer when the stomach is not full. If you are diabetic or need to eat/drink with your medication, get special instructions from your doctor.
Avoid any strenuous physical activity on the day of the test because you will need to exert yourself maximally if you are doing an exercise test.
Bring busy material. You will have periods of waiting throughout the test so bring a book, newspaper, knitting, etc. to keep you busy.
No smoking 4 hours prior to the test. Smoking may interfere with the test results.
Wear a comfortable two-piece outfit and comfortable shoes. A hospital gown may be provided and men may be asked to take off their shirt. Slacks or shorts are preferred if you are exercising. You should wear comfortable footwear appropriate for brisk exercise if you are doing an exercise test.
Do not wear oils or lotions before your test. Small sticky patches (electrodes) will need to stick to your chest.
Do not take the following heart medications on the day of your test unless your physician tells you otherwise or if the medication is needed to treat chest discomfort:
Isosorbide Dinitrate (for example: Isordil, Sorbitrate)
Isosorbide Mononitrate (for example: Ismo)
Nitroglycerin (for example: Deponit, Nitrostat)
Your physician may also ask you to stop taking other heart medications on the day of your test. If you have any questions about your medications, ask your physician.
NOTE: Do not discontinue any medication without first talking with your physician
What happens during the test?
When you enter the Stress Testing room, the Cardiology Tech/Nurse will have you sign
a consent form and he/she will make sure you understand the test. An IV will be started
in a vein in your arm. The Nuclear Medicine Tech will put your first injection of
Cardiolite through the IV. You will wait in the waiting room for at least 15 minutes
to let the Cardiolite circulate to your heart.
Once your waiting period is over, the Nuclear Medicine Tech will put you under the
camera for about 15 minutes. You will lay on your back on a table with your hand behind
your head. It is important for you to remain very still while the images are being taken.
The camera will move about you but never come in contact with you during the scan.
Following the completion of the scan, you will be escorted to a Stress Testing
room.
Exercise Cardiolite Stress Test
The patient is brought to the exercise laboratory where the heart rate and blood
pressure are recorded at rest. Sticky electrodes are attached to the chest and then
connected to the EKG portion of the Stress test machine with lead wires. A 12-lead EKG
is recorded on paper. Each lead of the EKG represents a different portion of the heart,
with adjacent leads representing a single wall.

The treadmill is then started at a relatively slow "warm-up" speed. The treadmill
speed and its slope or inclination are increased every three minutes according to
a preprogrammed protocol (Bruce is the commonest protocol in the USA, but several
other protocols are perfectly acceptable). The protocol dictates the precise speed
and slope. Each three minute interval is known as a Stage (Stage 1, Stage 2, Stage 3,
etc. Thus a patient completing Stage 3 has exercised for 3 x 3 = 9 minutes). The
patient's blood pressure is usually recorded during the second minute of each Stage.
However, it may be recorded more frequently if the readings are too high or too low.
Cardiolite is injected when maximum effort is achieved (Target heart rate). Sometimes
Cardiolite is injected sooner if indicated.
Indications would be if chest pain developed or if there was abnormal EKG tracings
that indicated coronary artery disease. After Cardiolite is injected, it is very
important to walk an additional minute for circulation. Treadmill will then be
terminated and then a recovery period of 5 minutes will be recorded.
Adenosine Cardiolite Stress Test
For patients who are unable to exercise adequately on the treadmill, the drug Adenosine may be given to produce an effect on the heart similar to exercise. During the test, you will be lying on the stretcher. The drug Adenosine will be infused through your IV. The Adenosine dosage you will be given is based on your body weight. Adenosine is a vasodilator so you may feel warm, flushed, experience chest pressure, headache, dizziness, nausea or shortness of breath. These symptoms are perfectly normal, but make sure to let the Cardiologist know how you feel. The Adenosine is infused over 5 minutes. Then you will be given another injection of Cardiolite three minutes into infusion. There will be a recovery period of at least 2 minutes after complete infusion of Adenosine.
What is Adenosine?
Adenosine is a coronary vasodilator that is used as a diagnostic agent in nuclear
Stress Testing. Adenosine works by increasing the blood vessel circumference of the
coronary arteries (arteries that feed the heart) in order to increase blood flow to
the heart. Adenosine causes a 20% increase in heart rate and a mild but significant
decrease in systolic and diastolic blood pressure. Adenosine is metabolized in the
liver. The amount of Adenosine you will be given is based on your body weight.
Side effects include: chest pain/pressure, dizziness, headache, nausea, dizziness,
shortness of breath, or a warm and flushed feeling. Adenosine is contraindicated in
patients who have a hypersensitivity to this drug. Adenosine can also cause bronchospasm
so your doctor may order a different test for you if you have a lung condition that
will be exacerbated by using Adenosine. Albuteral breathing treatment may be given
prior to and after Adenosine stress test.
Dobutamine Cardiolite Stress Test
For patients who are unable to exercise adequately on the treadmill, the drug Dobutamine may be given to produce an effect on the heart similar to exercise. During the test, you will be lying on the stretcher. A line of normal saline will be connected to your IV. The drug Dobutamine will be infused through your IV. The Dobutamine dosage you will be given is based on your body weight. Dobutamine is infused slowly through your IV, and the dose is increased every 3 minute. The Dobutamine infusion is turned off after it is infused for about 12 minutes.
The Dobutamine may be turned off early if:
You exceed a "target" heart rate based on your age
The Cardiologist or Cardio Tech/Nurse detects abnormal changes on your EKG
You experience significant symptoms, such as shortness of breath, chest pain, chest tightness, dizziness, etc. that do not permit you to exercise any longer.
Your blood pressure goes up too high
The dobutamine is infused longer than the 12 minutes if your heart rate has not
reached the predicted "target" heart rate. Sometimes the Cardiologist will have the
Nurse give you a drug called Atropine through your IV if your heart rate has not
sufficiently increased. You will be given one more injection of Cardiolite once
your heart rate is at or has exceeded your "target" heart rate.
Sometimes the Cardiologist will have the Nurse give you a drug called Lopressor
through your IV if your heart rate is taking a long time to decrease.
Lexiscan Cardiolite Stress Test
For patients who are unable to exercise adequately on the treadmill, the drug Lexiscan may be given to produce an effect on the heart similar to exercise. During the test, you will be lying on the stretcher. The drug Lexiscan will be infused through your IV. Lexiscan is a vasodilator so you may feel warm, flushed, experience chest pressure, headache, dizziness, nausea or shortness of breath. These symptoms are perfectly normal, but make sure to let the Cardiologist know how you feel. The Lexiscan is Injected within one minute followed by a saline flush. Another injection of Cardiolite will then be given immediately after Lexiscan followed by another saline flush. The Lexiscan stress test is completed in 4 minutes followed by a 2 minute recovery period. If symptoms have not subsided, another drug called Aminophyline may be given to reverse effects.

What is Carotid Ultrasound Imaging?
Ultrasound imaging, also called ultrasound scanning or
sonography,
involves exposing part of the body to high-frequency sound waves to produce pictures of
the inside of the body. Ultrasound exams do not use
ionizing radiation (as used in
x-rays).
Because ultrasound images are captured in real-time, they can show the structure and
movement of the body's internal organs, as well as blood flowing through blood vessels.
Ultrasound imaging is a noninvasive medical test that helps physicians diagnose and treat
medical conditions.
An ultrasound of the body's two carotid arteries, which are located on each side of the
neck and carry blood from the heart to the brain, provide detailed pictures of these
blood vessels.
A Doppler ultrasound study may be part of a carotid ultrasound examination.
Doppler ultrasound is a special ultrasound technique that evaluates blood as it flows
through a blood vessel, including the body's major arteries and veins in the abdomen,
arms, legs and neck.

What is EECP?
EECP is a mechanical procedure in which long inflatable cuffs (like blood pressure
cuffs) are wrapped around both of the patient’s legs. While the patient lies on a bed,
the leg cuffs are inflated and deflated with each heartbeat. This is accomplished by
means of a computer, which triggers off the patient’s ECG so that the cuffs deflate
just as each heartbeat begins, and inflate just as each heartbeat ends. When the cuffs
inflate they do so in a sequential fashion, so that the blood in the legs is “milked”
upwards, toward the heart.
EECP has two potentially beneficial actions on the heart. First, the milking action
of the leg cuffs increases the blood flow to the coronary arteries. (The coronary
arteries, unlike other arteries in the body, receive their blood flow after each
heartbeat instead of during each heartbeat. EECP, effectively, “pumps” blood into
the coronary arteries.) Second, by its deflating action just as the heart begins to
beat, EECP creates something like a sudden vacuum in the arteries, which reduces the
work of the heart muscle in pumping blood into the arteries. Both of these actions have
long been known to reduce cardiac ischemia (the lack of oxygen to the heart muscle) in
patients with coronary artery disease. Indeed, an invasive procedure that does the same
thing, intra-aortic counterpulsation (IACP, in which a balloon-tipped catheter is
positioned in the aorta, which then inflates and deflates in time with the heartbeat),
has been in widespread use in intensive care units for decades, and its effectiveness
in stabilizing extremely unstable patients is well known.
While a primitive form of external counterpulsation has also been around for a long
time, it has not been very effective until recently. Thanks to new computer technology
that allows the perfect timing of the inflation and deflation of the cuffs, and produces
the milking action, modern EECP has been greatly enhanced.
EECP is administered as a series of outpatient treatments. Patients receive 5 one-hour
sessions per week, for 7 weeks (for a total of 35 sessions). The 35 one-hour sessions
are aimed at provoking long lasting beneficial changes in the circulatory system.

What Are Peripheral Vascular Services?
Peripheral vascular services are non-invasive examinations of arteries and veins using ultrasound or Doppler. Tests include carotid duplex, venous duplex and arterial Doppler.
Who should have peripheral vascular examinations?
Patients who have symptoms of peripheral vascular disease or have recently experienced a stroke. Peripheral vascular services are often helpful in diagnosing peripheral vascular disease and looking for blockages or plaque in the arteries that may be the causes of stroke.
How often should you have peripheral vascular examinations?
As recommended by your physician.
How do you prepare for peripheral vascular procedures?
Generally, there is no preparation necessary for peripheral vascular procedures. However, your physician will give you any specific instructions if required.
What happens during the procedure?
The specifics will vary depending on the type of test. In most cases you will lie on your back while a water-soluble gel is placed on your skin over the extremity being tested. A hand-held transducer, which transmits high-frequency sound waves, will be passed over the area being tested. Often, blood pressure cuffs will be placed around your legs or arm depending on the type of test. The ultrasound or Doppler records images during this process.

Biventricular Pacemaker
(Also Called 'Cardiac Resynchronization Therapy', 'Device Therapy for Heart Failure')
What is cardiac resynchronization therapy?
Cardiac resynchronization therapy (CRT) is used to treat the delay in heart ventricle
contractions that occur in some people with advanced heart failure.
Heart failure means the heart’s pumping power is weaker than normal. With heart failure,
blood moves through the heart and body at a slower rate, and pressure in the heart
increases. A delay between the contraction of the right and left ventricles often occurs
with heart failure, so the walls of the left ventricle are unable to contract at the
same time.
The CRT pacing device (also called a biventricular pacemaker) is an electronic,
battery-powered device that is surgically implanted under the skin.
The device has 2 or 3 leads (wires) that are positioned in the heart to help the heart
beat in a more balanced way. The leads are implanted through a vein in the right atrium
and right ventricle and into the coronary sinus vein to pace the left ventricle.
How it works: When your heart rate drops below the set rate (programmed by your doctor),
the device generates (fires) small electrical impulses that pass through the leads to
the heart muscle. These impulses make the lower chambers (ventricles) of the heart
muscle contract, causing the right and left ventricles to pump together. The end result
is improved cardiac function.
CRT Device
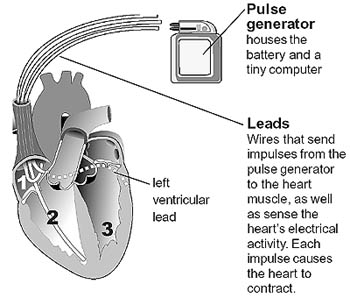
The CRT device (biventricular pacemaker) has 2 or 3 leads that are positioned in the:
Right atrium
Right ventricle
Left ventricle (via the coronary sinus vein)
Electrical system of the heart
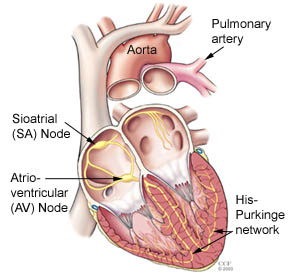
The atria and ventricles work together, alternately contracting and relaxing to
pump blood through the heart. The electrical system of the heart is the power source
that makes this possible.
Normally, the electrical impulse begins at the sinoatrial (SA) node, located in the
right atrium. The electrical activity spreads through the walls of the atria, causing
them to contract.
Next, the electrical impulse travels through the AV node, located between the atria
and ventricles. The AV node acts like a gate that slows the electrical signal before
it enters the ventricles. This delay gives the atria time to contract before the
ventricles do. From the AV node, the electrical impulse travels through the His-Purkinje
network, a pathway of specialized electricity- conducting fibers. Then the impulse
travels into the muscular walls of the ventricles, causing them to contract. This
sequence occurs with every heartbeat (usually 60-100 times per minute).
Benefits of CRT
CRT improves symptoms of heart failure in about 50% of patients who have been treated maximally with medications but still have severe or moderately severe heart failure symptoms. CRT improves survival, quality of life, heart function, the ability to exercise, and helps decrease hospitalizations in select patients with severe or moderately severe heart failure.
CRT and ICD therapy
Some patients with heart failure may benefit from a combination of CRT and an
implantable cardiac defibrillator (ICD). These devices combine biventricular pacing
with anti-tachycardia pacing and internal defibrillators to deliver treatment as
needed.
Of the patients who receive a biventricular device at Cleveland Clinic, about 90
percent receive a device that also provides defibrillator therapy. However, only
about 40 percent of the patients who receive defibrillators are also candidates
for a device that includes biventricular stimulation (CRT/ICD combination device).
The CRT/ICD combination devices:
Resynchronize the heartbeat
Slow down an abnormal fast heart rhythm
Prevent abnormally slow heart rhythms
Record a history of the patient’s heart rate and rhythm
Some CRT and ICD combination therapies have an internal monitoring device inside so
your doctor or nurse can track your heart rhythm and heart function, such as the
pressure in areas of your heart.
You may be asked to use a telephone to transmit data electronically from your device
to a computer server so your doctor or nurse can monitor your condition.
Is the device implant procedure safe?
A device implant is generally a very safe procedure. However, as with any invasive procedure, there are risks. Special precautions are taken to decrease your risks. Please discuss your specific concerns about the risks and benefits of the procedure with your doctor.
Will CRT improve my ejection fraction?
Yes, CRT can help improve your ejection fraction. Ejection fraction (EF) is the measurement of how much blood is being pumped out of the left ventricle of the heart. A normal EF ranges from 50% to 70%. People with heart failure who have a poor ejection fraction (EF less than 35%) are at risk for fast, irregular and sometimes life-threatening heart rhythms. The CRT/ICD combination device can help protect you against these dangerous, fast heart rhythms.
Success of CRT
Cleveland Clinic experience has shown that CRT improves patients’ ejection fraction by 5% to 10%. In some cases, patients with a CRT device develop normal ventricular function. Based on our experience, it is not rare for a patient to increase his or her ejection fraction over 40%.
Who is eligible to receive a CRT device?
People with heart failure who have a poor ejection fraction (< 35%) are at risk for fast, irregular and sometimes life- threatening heart rhythms. Ejection fraction is the measurement of how much blood is being pumped out of the left ventricle of the heart. CRT may be appropriate for people who:
have severe or moderately severe heart failure symptoms,
are taking medications to treat heart failure,
have delayed electrical activation of the heart (such as intraventricular conduction delay or bundle branch block), or
have a history of cardiac arrest or are at risk for cardiac arrest
Together, you and your doctor will determine if this treatment is right for you.
![]()
Home |
About Us |
Office
Locations | Procedures
Physicians |
Prevention |
Contact Us
The material provided on this site is for general
information purposes only.
It is not intended to be used as medical advice and does not substitute
for proper consultation with trained medical personnel.